Chris Reimer had never heard of Leopold, Mo., when he found himself rushing down a winding, two-lane road toward the rural, 65-person community in February.
Reimer, a social media manager in St. Louis, had made a split-second decision when he saw a local television reporter tweet about a 2,000-dose COVID-19 vaccination clinic opening to anyone after 3 p.m. that day.
"I jumped in the car and started driving south," Reimer says, though the clinic was two hours away in Leopold. "I definitely saw other cars [on the interstate highway] and thought to myself, 'I wonder if they're going the same place I am?' because we were all driving perhaps a little too quickly."
Reimer arrived just before the clinic's 5 p.m. cut-off time, and says he was thrilled when National Guardsmen running the clinic filled out his vaccine card.
"This is really happening! I am getting the vaccine," he recalls thinking, along with a pang of guilt. At 50 years old, Reimer didn't belong to any priority groups eligible for vaccination at that time in Missouri.
The Bollinger County Health Center, which put on the event with the National Guard, considered it a success, though over 1,000 doses went unused at that day's clinic, and others went to urbanites like Reimer, willing to make a long drive to get their shot.
Early in the vaccine rollout, advocacy groups like the National Rural Health Association urged states to focus more resources toward rural areas like Leopold, which generally have older, less healthy populations and fewer health care options.
And some rural communities have done well, with COVID-19 vaccination rates that equal or exceed urban communities in their states.
But, an NPR analysis of county-level vaccination data from the Centers for Disease Control and Prevention shows signs of an emerging rural-urban divide.
When looking at vaccination rates of all adults 18 and older, rural counties appear to have largely kept pace with their urban counterparts, with rural rates on average landing within 5 percentage points of urban rates in most states.
However, among people who are 65 years old or older, the gap between rural and urban counties is wider in most states. Urban counties' vaccination rates outpace rural ones in all but seven states for which there's complete data. In 17 states, urban rates exceed rural rates by 5 or more percentage points.
Widening gaps
The wider gaps in vaccination rates among senior citizens could foreshadow a brewing rural-urban divide, several experts told NPR.
"It would suggest that we're potentially starting to see that trend [of rural/urban disparities] emerge because older adults, by and large, have had the opportunity to get vaccinated at this point," says Timothy Callaghan, a health policy researcher from Texas A&M University's Southwest Rural Health Research Center.
That leaves only the more vaccine-hesitant behind, Callaghan adds. In other words, the vaccination rates seen in seniors may very well presage vaccination rates that could be expected among all adults, once younger adults have had similar opportunities to get their shots.
In some cases, data shows these rural-urban gaps are significant. Nebraska, Massachusetts and Louisiana have the largest gaps among seniors, with rural Nebraskan counties averaging about 19 percentage points behind the state's urban counties.
NPR's analysis reveals the gaps are already growing in some places. Urban counties in Missouri, Pennsylvania and Kansas all widened their lead over rural counties by more than 5 percentage points among seniors in the three weeks the CDC has been releasing daily county-level updates.
"It's troubling, especially because that older population makes up a greater percentage of rural counties," says Tim Marema, editor of the Daily Yonder, a news site published by the Center for Rural Strategies. "The more elderly population has been eligible for the vaccine for a longer period of time, so you would expect to see rural even, [or] maybe a little bit ahead."
And smaller, yet noticeable changes are beginning to show up in vaccination rates for the general population, as Callaghan predicted. Three-quarters of states have seen urban rates for all ages grow slightly faster than rural rates since the end of March, widening the rural-urban gap by 4 percentage points in both North Dakota and Florida since the end of March.
The reasons for the gaps are likely a mixture of hesitancy, access and messaging issues. Rural Americans are 11 percentage points more likely than city-dwellers to say they will definitely not get a COVID-19 vaccine, according to Kaiser Family Foundation polling out this month.
Callaghan says his own research shows people living in rural communities are significantly less likely to take preventative measures against COVID-19, including wearing face masks and avoiding restaurant dining.
"Where there's more rural Americans who aren't following these guidelines, that potentially leads to the need for more health messaging, so you can avoid negative outcomes," Callaghan says.
When it comes to what actually makes people resist vaccination, Callaghan contends political ideology plays a stronger role than geography.
"There's more conservative individuals in rural areas, and those conservative individuals are less likely to vaccinate," he says.
Outside of vaccine hesitancy, Callaghan points to fewer health care providers, poor transportation options and language barriers among migrant workers as vaccination roadblocks for rural counties.
What's working in rural areas
Despite the troubling trends, there are some bright spots in NPR's analysis of rural vaccination rates.
Rural counties in Arizona and Alaska have held sizable leads over urban counties since the end of March, when examining vaccination rates for the entire population, and rural counties in a handful of states like Wyoming, New York and Oregon have even gained a point or two over urban counterparts since the end of March.
Experts say some aspects of rural life — including the close-knit nature of smaller towns — may in fact lend themselves to successful vaccination campaigns.
One notable success is Santa Rosa, N.M. Two hours east of Albuquerque with a population of 2,600, Santa Rosa has just one 10-bed hospital and a lone pharmacy serving the surrounding Guadalupe County.
By mid-February, though, the county had vaccinated over 40% of residents 16 years and older, while most other counties nationwide still had vaccination rates barely out of the single digits.
"When our numbers got publicized statewide, and raised a lot of eyebrows, we were kind of informed [by the state], 'OK, hold off. You're way ahead of everybody else. We're going to hold you back for a while,' " says Christina Campos, administrator of the Guadalupe County Hospital.
Campos credits her small county's sense of community for allowing them to take an early lead in the vaccination race and maintain New Mexico's highest county vaccination rate even today, three months later.
"When they say it takes a village, this really, really took the entire village," Campos says of their 900-person vaccination drive in January at the local high school gym.
The hospital's single pharmacist drew up all 898 shots, hospital staff and volunteers from the city, county and school district all kept lines moving, and local businesses donated meals.
Residents of Guadalupe County have been eager for the vaccine, Campos says, adding the hospital continues to administer about 100 shots per week. She attributes this to the fact the county has lost nine people – many of them young – to COVID-19. After that, she says, "The risk of COVID was no longer anecdotal. It was front and center."
Campos also credits the simple fact that a hospital exists in the area for helping Guadalupe County get out in front of vaccination so early. She listed four rural counties in New Mexico without a single hospital to spearhead local vaccination efforts, and all four currently trail behind New Mexico's average county vaccination rate.
Keith Mueller, director of the Rural Policy Research Institute at the University of Iowa, has been encouraging decision-makers to look beyond hospitals and chain pharmacies to get vaccines delivered to more rural communities.
"If you get the doses out there, to a known provider, you can get them distributed," Mueller says. "There is a strong network even within the small [rural] counties, and they can do what you just described in New Mexico. Give them 900 doses; they'll get those 900 doses administered within the timeframe of the life expectancy of the medication."
Mueller suggests states could provide a traveling workforce, perhaps of students from local pharmacy schools, to lead vaccine clinics in rural areas where a local clinic might not be able to spare staff from day-to-day operations.
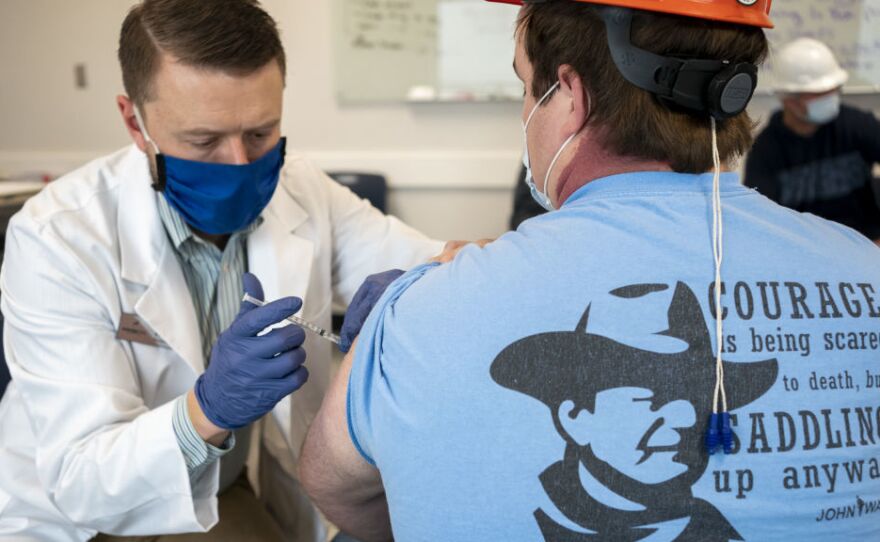
Several states have deployed National Guard troops as that traveling workforce, and the Federal Emergency Management Agency has sent 10 mobile units to vaccinate hard-to-reach areas of states like Colorado, Maine, and Nevada in the past few weeks. Many of FEMA's roving clinics rely on the one-shot Johnson & Johnson vaccine, however, which means they've been halted temporarily following concerns about rare blood clotting disorders the CDC announced last week.
But even with added manpower from state governments and FEMA and infusions of federal cash, rural clinics don't always go to plan — or find a lot of takers, as Chris Reimer discovered in Missouri.
Anecdotally, urban residents from Minnesota to Tennessee to the District of Columbia have been making drives like Reimer's to track down vaccines in rural areas, yet the opposite has proven true elsewhere. Fifteen remote, rural counties in Texas have yet to receive a single dose of COVID-19 vaccine, but state data shows at least a quarter of each of these small counties' residents aged 16 and older have taken at least one dose.
"What's clear here is that there is no consistent pattern across the country," says Callaghan, the Texas A&M researcher. "In certain states, rural communities are doing very well, and other states, rural communities aren't doing very well."
For the rural places that have fallen behind, Marema of the Center for Rural Strategies challenged civic groups and religious organizations to dig into their well-established networks to win over the hearts and minds of the vaccine-hesitant.
"In rural America, in the Christian tradition, we take care of sick people. That's a command," Marema says. "I know it's politicized, but I think people have got to get a grip on the reality of what we are facing, and what the impact is on the people we love. If we love our community and we love each other, we have to get that vaccine."
Methodology
Data used for this story comes from county-level counts of fully vaccinated people updated daily by the Centers for Disease Control and Prevention. The CDC has not released data for Texas, Hawaii and California's smallest counties. NPR excluded seven states where less than 80 percent of vaccination records included a person's county of residence.
NPR coded each county as rural or urban according to the National Center for Health Statistics 2013 Urban-Rural Classification Scheme, marking non-core and micropolitan counties as rural and small, medium and large metro counties as urban. NPR excluded Delaware, the District of Columbia, New Jersey and Rhode Island because they have no rural counties and Puerto Rico because the NCHS scheme does not classify its municipios.
For the remaining 38 states, NPR used 2019 Census population estimates for county residents aged 18+ and 65+ to calculate the average vaccination rates for each state's rural and urban counties, weighted by county population.
Copyright 2021 NPR. To see more, visit https://www.npr.org.