Della McCullough has been struggling with her weight since she was 11, when she remembers her mother telling her she was "big boned." Now 53, she says she's tried supplements, diet and exercise — even an all-fruit diet once. None of them worked.
"Still, I'm not doing well," says McCullough, a semiretired school bus driver in Colorado. "I have done nutrition counseling, trauma counseling, meditation, positive affirmation therapy, and still I am almost 300 pounds again and sad and unhappy."
She is interested in new blockbuster drugs that help people with overweight and obesity.
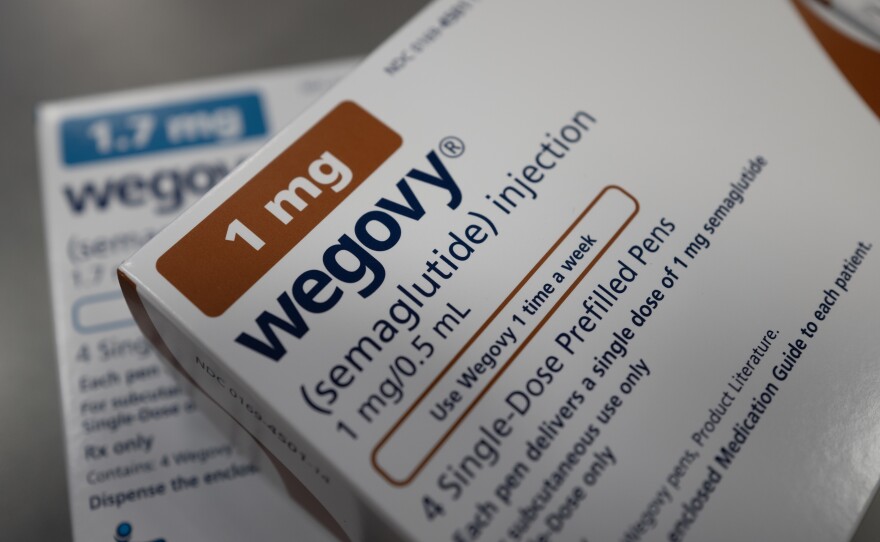
But she and her husband found themselves on Medicaid for the first time last year. Colorado's Medicaid plan won't cover Wegovy for her, an obesity medicine made by Novo Nordisk that she'd like to try.
Wegovy contains the same active ingredient as Novo Nordisk's Ozempic, a diabetes drug, but Wegovy is specifically approved for obesity and weight loss.
An old law complicates Medicaid coverage
Medicaid doesn't have to cover Wegovy and drugs like it because of a decades-old law excluding medicines that treat anorexia, weight gain and weight loss from required coverage.
McCullough is frustrated. "I'm not ashamed of the fact that I am on state assistance, and I can say that what assistance they provide is not adequate, especially if you do have obesity," McCullough says.

Robin Feldman, a professor at the University of California Law in San Francisco, says when the law excluding weight-related drugs was passed in the 1990s, everyone thought diet and exercise were the key to losing weight and keeping it off — even though the evidence doesn't support that. "So in that context, being overweight was viewed as lacking willpower and dedication."
While state Medicaid programs don't have to cover weight loss drugs, 16 do right now.
Cost is a factor limiting coverage. Wegovy's list price is more than $1,300 dollars a month. Even if Medicaid programs get a big discount, which they typically do, the total spending could be significant.
Researchers at Brown University found that people on Medicaid are 27% more likely to have obesity compared with people who have commercial insurance.
And people may take these drugs for years.
"States are always having to grapple with, you know, this investment or that investment," says Kate McEvoy, executive director of the National Association of Medicaid Directors. "There are a lot of other preventive health issues, notably around maternal health, issues for children. And so examining the relative merits of those investments is kind of where states are right now."
More Medicaid plans are considering Wegovy
Some state Medicaid programs, like Minnesota's, cover Wegovy because they're required to under state law. Others, like Louisiana's, don't cover Wegovy at all but cover an old weight loss drug, Orlistat, which is considered less effective.
In North Carolina, Kody Kinsley, the state's Secretary of Health and Human Services says he hopes the Medicaid program will cover Wegovy by this summer.
"We have a kind of a standard policy process," he says. "We go through to consider the actuarial impacts, the negotiation of rebates, the value of adding the drugs, all of which we don't really go through for any other drug because they're required to be covered. But for these, because of that federal carve out, we are going through that process."
He says Wegovy would not be the most expensive drug North Carolina's Medicaid program covers and won't bankrupt it.
Advocates say policies that exclude treatments to help people lose weight need to change. "Research shows us that obesity is a complex chronic disease," says Tracy Zvenyach, director of policy strategy and alliances at the Obesity Action Coalition, a national nonprofit organization that is trying to expand access to evidence-based treatments for obesity. "The science is clear that obesity is driven by powerful biology, not by choice," Zvenyach says.
In Colorado, where McCullough lives, Medicaid doesn't cover Wegovy for weight loss.
However, Wegovy was recently approved by the Food and Drug Administration to reduce risk of cardiovascular death, heart attack and stroke for people with cardiovascular disease and who are overweight or obese. That means Medicaid would be required to cover it for some people since it's not just a weight loss drug anymore.
"In Colorado, Wegovy is currently covered by Colorado Medicaid when it's used to reduce the risk of major cardiovascular events in adults with established cardiovascular disease and either obesity or overweight as approved by the FDA," says Marc Williams, a spokesman for the Colorado Department of Health Care Policy and Financing.
But McCullough doesn't have cardiovascular disease and wouldn't qualify.
She says people with obesity are treated differently from people with other health conditions. I ask her if that felt personal.
"You know, I never would have thought that, but now that I'm in that situation, it does feel very personal," she says. "Like, 'She's just fat,' you know? 'It's her problem. She'll figure something out.' Or 'She'll need to change whatever she does.' "
She hopes the policies eventually catch up to the science.
Copyright 2024 NPR. To see more, visit https://www.npr.org. 9(MDAzMjM2NDYzMDEyMzc1Njk5NjAxNzY3OQ001))