IF PRESENT TRENDS ARE NOT REVERSED, THE CENTERS FOR DISEASE CONTROL SAYS AS MANY AS ONE IN THREE AMERICANS WILL HAVE DIABETES BY THE YEAR 2030. NOW THE CDC AND MEDICARE ARE WORKING TOGETHER ON A NEW PROGRAM THEY HOPE WILL REDUCE THOSE NUMBERS. STARTING NEXT JANUARY, THE MEDICARE DIABETES PREVENTION PROGRAM WILL PAY $450 TO DOCTORS AND OTHER CARE PROVIDERS WHO CAN GET PRE-BITE -- DIABETIC BENEFICIARIES TO LOSE WEIGHT AND TAKE A YEAR-LONG HEALTH CLASS. THE HOPE IS THAT PARTICIPANTS WILL AVOID DEVELOPING THE DISEASE AND SAVE BILLIONS OF DOLLARS AND HOSPITALIZATION AND OTHER DIABETES RELATED CAUSES. JOINING ME AS DR. ATHENA PHYLLIS AMICUS VICE PRESIDENT OF THIS DIABETES INSTITUTE. WILL COME TO THE PROGRAM. HELLO, THANK YOU FOR HAVING ME. YOU HAVE A TRIAL WITH 100 PREDIABETIC PATIENTS. IS YOUR PROGRAM BASICALLY WHAT THIS MEDICARE PROGRAM WOULD LOOK LIKE? IT IS EXACTLY A RECORD APPLICATION -- AN EXACT REPLICATION. SO THE PATIENTS ARE OLDER, ON MEDICARE, HOW DO YOU GO ABOUT BREAKING THE DIET AND EXERCISE HABITS OF SOMEONE WHO MAY NOT HAVE CHANGED IN DECADES? IT'S A GREAT QUESTION, IT'S PROBABLY ONE THAT WE HAVE BEEN TRYING TO FIGURE OUT FOR A LONG TIME. THE YEAR-LONG APPROACH IS MOST IMPORTANT HERE. IN THE FIRST FOUR MONTHS, PATIENTS ARE SEEN EVERY WEEK. THEY HAVE TO BE MOTIVATED AND COMMITTED. IF THEY PASS THE SCREENING, FOUND TO BE AT RISK, THEY HAVE TO BE WILLING TO COME IN EVERY WEEK AND IN THOSE FIRST FOUR MONTHS, THEY ARE BEING TAUGHT AND PUT INTO PRACTICAL USE IN THAT TIME PERIOD BETWEEN THE WEEKS, EVERYTHING THEY LEARN. INCREASING PHYSICAL ACTIVITY, CHANGING THE FAT IN THEIR DIET, THE PORTIONS, BUT FOUR MONTHS IS A FAIRLY LONG PERIOD OF TIME TO PRACTICE MAKING CHANGES. THEREAFTER, THEY COME IN ONCE A MONTH FOR A FULL YEAR TO MAINTAIN THE HABITS THEY HAVE LEARNED. IT WAS DEMONSTRATED IN THE DIABETES PREVENTION PROGRAM AND THE OFFICIAL STUDY A FEW YEARS AGO THAT IT WAS ENOUGH TO HAVE PEOPLE CHANGE THEIR HABITS AND ACHIEVE WEIGHT LOSS. THE GOAL OF THE PROGRAM IS TO GET PATIENTS TO REDUCE THEIR WEIGHT BY 9%. THEN SHOW UP FOR THE CLASSES YOU HAVE BEEN TALKING ABOUT. WHAT KIND OF SUCCESS HAS YOUR PROGRAM HAD WITH WEIGHT LOSS AND PEOPLE SHOWING UP REGULARLY FOR CLASSES. WE HAVE HAD GOOD SUCCESS. MOSTLY DUE TO THE FACT THAT YOU SCREEN PEOPLE UP FRONT AND PEOPLE HAVE TO UNDERSTAND WHAT THEY ARE GETTING INTO. WE HAVE BEEN ABLE TO ACHIEVE MORE THAN 75% OF THE POPULATION TO STAY IN FOR THE TIME PERIOD, THE WEIGHT LOSS IS SOMETHING WE HAVE NOT GONE OUT ONE YEAR. WE DON'T KNOW WHAT THE ACTUAL WEIGHT LOSS PERCENTAGE WILL BE BUT WE ARE SEEING SOME NICE SUCCESSES, THAT CAN RANGE FROM 5%-20% DROP IN SOME PATIENTS. DOCTORS WOULD GET $450 PER PATIENT UNDER THIS NEW PROGRAM. IF THE PATIENTS SUCCEED IN FULFILLING THE REQUIREMENT, I KNOW YOU HAVE SAID YOU ARE WORRIED, IT MIGHT NOT BE ENOUGH TO PAY FOR THE DOCTORS OR HEALTHCARE PROVIDERS COSTS, HOW MUCH IS IT COSTING YOU? THE WAY WE CONDUCT IT IS WE HAVE EDUCATORS, DON'T USE PHYSICIANS TO CONDUCT THIS WE HAVE COACHES WHO HAVE BEEN TRAINED TO DO THIS. THAT IS A LEANER AND MEANER WAY TO CONDUCT THE PROGRAM, THEY ARE WELL EDUCATED AND HOW TO PERFORM AND ACHIEVE OUTCOMES WE WANT TO ACHIEVE. BUT WE DO NEED TO MAKE SURE WE CAN EMPLOY THEM FOR THAT ENTIRE PERIOD OF TIME. SO, IT IS COSTING US A LITTLE MORE THAN THE 450 PER PARTICIPANT. WE HAVE TO MAKE SURE WE HAVE A FULL CLASS, IN ORDER TO MAKE IT ACHIEVABLE. IT'S NOT JUST DOCTORS WHO CAN GET PAID BY MEDICARE OR THIS. AT LEAST, PEOPLE WHO HAVE APPLIED, ENTITIES WHO HAVE APPLIED FOR THIS, INCLUDE SUPERMARKETS, JENNY CRAIG, CHURCHES, ARE YOU ENCOURAGED AT HOW WIDESPREAD THIS COULD BE? OR, A LITTLE WARY THAT ALL THESE ENTITIES MAY NOT BE UP TO THE TASK? THAT'S INTERESTING, I AM ACTUALLY ENCOURAGE. I THINK THE MORE BROADLY WE CAN SPREAD THIS, WE NEED AN ARMY TO GET OUT THERE AND SPREAD THE WORD ON WHAT NEEDS TO BE DONE. THE ONLY CONCERN I HAVE IS THE PEOPLE WHO ARE DOING THIS ARE WELL TRAINED TO DO IT. THERE IS A CERTAIN CURRICULUM THAT NEEDS TO BE FOLLOWED AND YOU NEED THE RIGHT INFORMATION TO BE CONVEYED TO THE PARTICIPANTS, NOT MISS INFORMATION. AS LONG AS THERE IS STANDARD OR CRITERIA FOR ENSURING THE COACHES CONDUCTING THIS ARE DOING IT THE RIGHT WAY, THEN ABSOLUTELY. THE MORE THE BETTER. THIS NEEDS TO BE SPREAD THROUGHOUT THE ENTIRE COUNTRY. DR., IS SAN DIEGO SEEING THE SAME RIGHTS AND DIABETES AS THE REST OF THE NATION? NOT ONLY IS IT SEEING THE SAME KIND OF RICE IT IS SAYING MORE. BECAUSE OF OUR MIX OF THE LATINO POPULATION, RETIREE POPULATION, THOSE ARE BOTH HIGH RISK FOR DEVELOPING DIABETES. THE RATES IN SAN DIEGO ARE HIGHER THAN THE REST OF THE NATION. THE FINAL RULES FOR THIS PROGRAM, DUE OUT IN THE NEXT WEEK. WHAT ARE YOU GOING TO BE PAYING CLOSE ATTENTION TO IN TERMS OF POTENTIAL CHANGES? I THINK FOR ME, THE ONE I AM LOOKING FOR IS WHAT THEY ARE EXPECT FOR WEIGHT LOSS. YOU MENTIONED IN THE BEGINNING, 9%, THAT IS WHAT THEY PUT OUT BUT THEY ASKED FOR RESPONSES ON WHETHER THOSE OF US DOING THIS THING FIZZES -- THINK THIS IS ACHIEVABLE. MOST HAD A 5-7% AND THAT HAD A 58% REDUCTION IN THE DEVELOPMENT, I THINK THAT IS MORE REASONABLE. IT IS VERY HARD TO ACHIEVE THE 9% SUSTAINED WEIGHT LOSS. I WOULD HOPE THERE MIGHT BE A LITTLE BIT LOWER GOLD FOR THAT. IS THIS WHOLE PROGRAM SUBJECT TO BEING CUT DURING HEALTHCARE REFORM? I GUESS WE DON'T KNOW WHAT WILL BE CUT IN THE LONG TERM. I WOULD HOPE NOT, YOU STARTED OUT AT THE BEGINNING TALKING ABOUT HOW MANY PEOPLE HAVE PRE-DIABETES IN THIS COUNTRY AND DIABETES, THE COSTS, ARE ENORMOUS. IF THERE IS ANYWAY WE CAN HELP STEM THIS COST AND DISEASE, IT WOULD BE INCREDIBLY VALUABLE IN MANY WAYS. I HAVE BEEN SPEAKING WITH DR. ATHENA AMICUS. DR. THANK YOU SO MUCH. THANK YOU
Oscar and Teri Lara of Rancho Bernardo were diagnosed with prediabetes a few months ago, a condition 86 million Americans share.
That means the retired couple lives with a greater chance they will develop diabetes, which can lead to heart, nerve, kidney and eye disease, and an early death.
The Laras are lucky. Nine in 10 Americans do not know they have prediabetes, but the Laras were caught early. They have an opportunity to alter their diets, reduce their sugar intake and lose weight, and likely postpone or prevent that trajectory.
On advice from their doctors, they enrolled in a special lifestyle class, part of the Scripps Diabetes Prevention Program, much like the curriculum that will be offered to Medicare beneficiaries across the country, free of charge, starting Jan. 1.
“This class changed my thinking about what I eat, how much I eat, how to stay focused, and how to maintain a healthy regimen of proper nutrients to put into my body,” Oscar Lara said. Instead of chomping down on bread and burritos, it’ is broccoli, Brussels sprouts and salads.
$450 for a few pounds of flesh
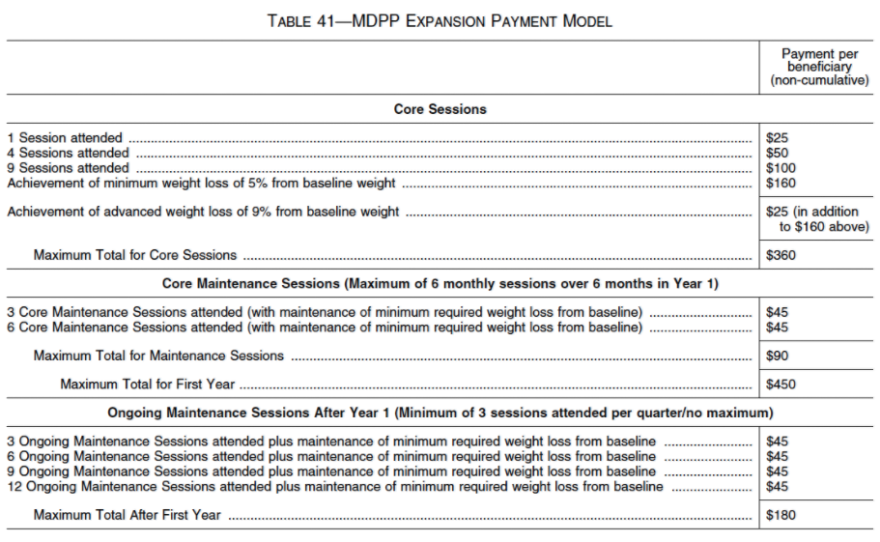
Providers who run Medicare’s year-long programs will receive up to $425 per participant if attendees take all the classes and lose 5 percent of their body weight during the year; $450 if they lose 9 percent. If attendees miss classes, drop out, or fail to lose that much — or gain it back — the programs will be paid incrementally less.
In 2012, the direct medical costs for 29 million people diagnosed with diabetes in the U.S. was an estimated $176 billion, including hospital, drug, and physician services. That is why the issue is so critical and why the agency that runs Medicare wants to put a dent in that spending.
After all, 21 percent of patients with diabetes are Medicare eligibles diagnosed after they turn 65.
Numerous studies going back 16 years have shown that people can delay or prevent diabetes by losing weight; a drop of a few pounds improves the body’s ability to manage sugar intake.
Looking out for fraud
The Centers for Medicare and Medicaid Services (CMS) has made it clear it will be looking for cheaters: those providers who enroll people without documented prediabetes, or who falsify weight loss or attendance. CMS can track much of that through inconsistencies in subsequent billing. It referenced the word “fraud” 13 times in the latest rules for the program.
But federal officials believe the program is worth the risk because weight loss in a population with prediabetes has the potential to save that much more money.
For Ann Albright, PhD, RD, director of the diabetes program at the Centers for Disease Control and Prevention (CDC) which is helping to write the program’s rules, said the incentive payments are long overdue.
“We have a medication distribution system in this country, but not a lifestyle distribution system, and that’s what this program is going to do,” she said.
Dr. David Nathan, a Massachusetts General Hospital diabetes expert whose 2002 study proved the lifestyle intervention concept works, called the program “extremely extraordinary.”
Researchers in his multicenter study randomized thousands of overweight people with prediabetes. They were divided into three groups. One third received a series of individualized lifestyle sessions, one third received the drug metformin, which controls blood sugar levels, and one-third received no intervention.
The result? Lifestyle intervention not only resulted in greater weight loss, but it also delayed or prevented many people from progressing to diabetes, and had an even greater beneficial impact on seniors.
“We know our program works,” Nathan said.
Churches and supermarkets
Some 1,425 settings — including 13 in San Diego County — have applied for certification. They include hospitals systems, physician practices and clinics, pharmacies, wellness centers, hospital systems, county governments, Jenny Craigs, and even churches and Albertson’s supermarkets.
CDC diabetes communications specialist Josh Petty said many others are being processed to meet what is hoped to be a huge national demand.
The centers must have CDC certification, but the rules to date do not specify how instructors should be trained.
Diabetes prevention programs have used federal grants or private insurance in the past. The YMCA-USA version used an $11 million federal grant to enroll 7,000 Medicare beneficiaries in eight states for a three-year program. It realized savings of $278 per person in costs for hospitalizations and emergency room visits.
But the new program is the first to tackle all Medicare beneficiaries with blood glucose levels indicating prediabetes and who have a BMI of at least 25, or for Asians, at least 23.
Is the money enough?
It is hard to get some people to schedule time or feel comfortable discussing weight gain and intimate health problems in group settings. And many physicians worry that programs will fall apart if patients do not enroll and stick to the plan.
Oscar Lara had a lot of incentive. Awhile back, he had a stroke, and has survived cancer. “Prior to this program, I felt I could eat whatever I wanted. Sugar, carbohydrates, the things that spike glucose,” he said. “Now this class has kept me focused. It’s really been a lifestyle change.”
Athena Philis-Tsimikas, MD, vice president of the San Diego-based Scripps Diabetes Care and Prevention program in La Jolla, is optimistic, and now is running a year-long trial program with 100 participants, which the Laras now attend.
But she is frankly worried that $450 will not pencil out to hire enough staff to support, phone and remind participants, and there is data collection and submission requirements too.
“There’s a lot of ifs in this,” she said. And it’s hard to tell right now, with $450 per participant, if we’re going to be able to do that. It would mean we would have to run a really lean operation.”
San Diego endocrinologist Dr. Paul Speckart thinks the best way to get people to lose weight to prevent diabetes is to pay them directly.
“It’s almost an article of faith that talking and lectures don’t work to get patients to lose weight,” he said “People don’t. We almost always have to move to pharmaceutical solutions.”
What might be more effective, he said, is to give people with prediabetes brochures about diet and exercise, but pay them $200 every month their observed weight drops another 1 percent from baseline for a year. His rule: Failure in any one month would get them expelled.
More patients screened
A key to success of the program is to ensure that physicians aggressively screen Medicare beneficiaries for prediabetes.
People who read their blood test results should look for a fasting glucose of 100 and 125 mg/dL or an A1c between 5.7 and 6.4 percent to see if they have prediabetes.
A element critical to the program is that doctors explain the the seriousness of the condition and refer patients. Counseling people to lose weight is not something doctors like to do, and some question whether they would be paid for the extra time.
But Elizabeth Joy, MD, clinical champion for the Intermountain Diabetes Prevention Program at Intermountain Health in Salt Lake City, said she thinks physicians should welcome the extra help to support at-risk patients to lose weight.
“It’s pretty unethical to screen people for a condition for which we have no treatment,” she said. “Now we actually have a treatment with proven efficacy.”
Doctors can keep it simple, saying that based on a patient’s weight and testing, they scored as high risk. “You scored a 10. I would like you to go to this program, and my care manager is going to help set that up.”
Dr. R. James Dudl, a diabetes expert with Kaiser Permanente Research in San Diego, said patients who develop prediabetes should get the word directly from their physician in person, rather than from a staff person. That conveys the urgency of the situation, he said, advising physicians, “Doctor, you do not get off the hook.”
American Diabetes Association president-elect Dr. Jane Reusch is hopeful this program can work.
A variety of prevention programs have been tried, with or without insurance payments, copayments and deductibles, and federal and state funding, she said.
“But a lot of them fail to stick because there hasn’t been a carrot there. Now, with $450, there’s a monetary resource.”
For the Laras, the program has gotten results.
Oscar Lara goes to the gym three times a week, plays softball and golf, and has lost 35 pounds. And vegetables and lean meats have replaced a lot of the carbohydrates he and his wife used to eat. The sugar levels in his blood are back to normal range.
Teri Lara has also lost weight and she walks every day as much as arthritis permits.
“I’m not on a diet,” Oscar Lara said. “I’ve just changed the way I look at things and changed the way I look at food.”






