Approaching a van that distributes safe supplies for drug use in Greenfield, Mass., a man named Kyle noticed an alert about xylazine.
"Xylazine?" he asked, sounding out the unfamiliar word. "Tell me more."
A street-outreach team from Tapestry Health delivered what's becoming a routine warning. Xylazine is an animal tranquilizer. It's not approved for humans, but it's showing up in about half of the drug samples that Tapestry tests in the rolling hills of western Massachusetts. It's appearing mostly in the illegal fentanyl supply but also in cocaine.
Kyle rocked backward on his heels at the mention of cocaine. He and his friends regularly use cocaine, but lately, they had suspected that something else was in the bag.
"The past week, we've all been just racking our brains, like 'What is going on?'" he said. "Because if we cook it up and we smoke it, we're falling asleep after."
(NPR and KHN are using first names in this story for people who use illegal drugs.)
Kyle's deep sleep might have been triggered by fentanyl too, but Kyle said one of his buddies used a test strip to check for the opioid and none was detected.
Xylazine surged first in some areas of Puerto Rico and then in Philadelphia, where it was found in 91% of opioid samples last year, the most recent reporting period. Data from January to mid-June shows that xylazine was in 28% of drug samples tested by the Massachusetts Drug Supply Data Stream (MADDS), a state-funded network of community drug-checking and advisory groups that uses mass spectrometers to let people know what's in bags or pills purchased on the street.
Some areas of the state, including western Massachusetts, are seeing xylazine in 50% to 75% of samples. In Greenfield, that's a big change from last year, when xylazine wasn't a concern.
"We've seen an exponential increase during the pandemic," said Traci Green, who oversees MADDS and directs the Opioid Policy Research Collaborative at Brandeis University. "Now the sad thing is we're really seeing it all over the state. It's definitely hazardous."
There's a lot of speculation about how and why xylazine is on the rise. It may be added to fentanyl or heroin to help extend the effects of an opioid high. Dealers also may be using this relatively inexpensive and easy-to-order sedative because of supply chain gaps with other drugs.
Whatever its path into the drug supply, the presence of xylazine is triggering warnings in Massachusetts and beyond for many reasons.
As xylazine rises, overdoses rise too
Perhaps the biggest concern is an association with more overdoses and deaths. In one study of 10 cities and states, xylazine was detected in fewer than 1% of overdose deaths in 2015, but in 6.7% in 2020, a year the U.S. set a new record for overdose deaths. That record was broken again in 2021 with more than 107,000 deaths.
The study does not claim xylazine is causing more fatalities, but study co-author Chelsea Shover said it may contribute. Xylazine, a sedative, slows breathing and heart rate, as well as decreases blood pressure, compounding some effects of an opioid like fentanyl or heroin.
"If you have an opioid and a sedative, those two things are going to have stronger effects together," said Shover, an epidemiologist at UCLA's School of Medicine.
In Greenfield, Tapestry Health is responding to more overdoses as more tests show the presence of xylazine.
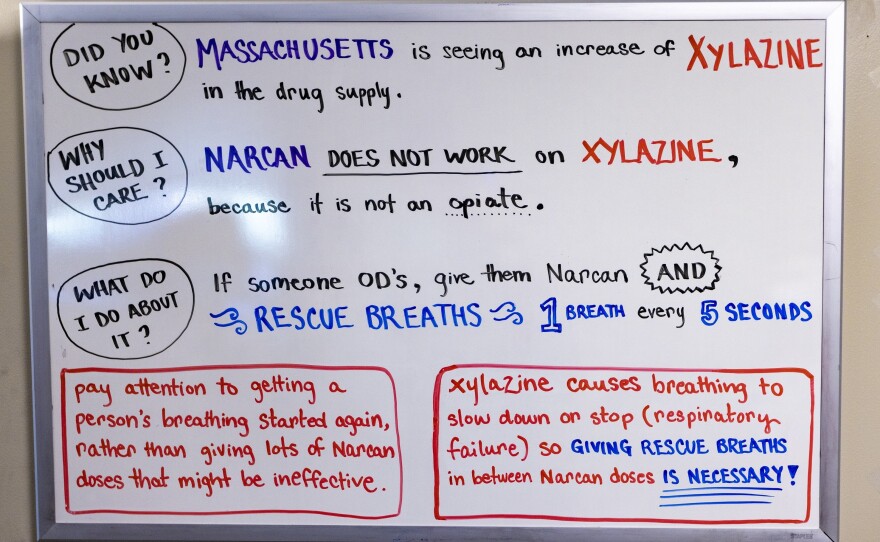
"It correlates with the rise, and it correlates with Narcan not being effective to reverse xylazine," said Amy Davis, the assistant director for rural harm-reduction operations at Tapestry. Narcan is a brand name of naloxone, an opioid overdose reversal medication.
"It's scary to hear that there's something new going around that could be stronger maybe than what I've had," said May, a woman who stopped by Tapestry's van. May said she has a strong tolerance for fentanyl, but a few months ago, she started getting something that didn't feel like fentanyl, something that "knocked me out before I could even put my stuff away."
A shifting overdose response
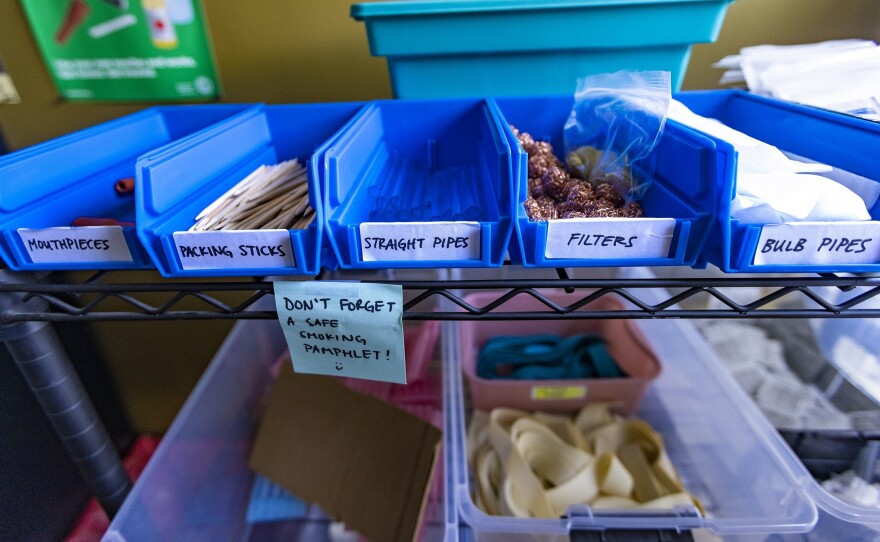
Davis and her colleagues are ramping up the safety messages: Never use alone, always start with a small dose and always carry Narcan.
Davis is also changing the way they talk about drug overdoses. They begin by explaining that xylazine is not an opioid. Squirting naloxone into someone's nose won't reverse a deep xylazine sedation — the rescuer won't see the dramatic wake-up that is more common when giving Narcan after an opioid overdose.
With xylazine, the immediate goal is to make sure the person is getting oxygen into the brain. So Davis and others advise starting rescue breathing after giving the first dose of Narcan. It may help restart the lungs even if the person doesn't wake up.
"We don't want to be focused on consciousness — we want to be focused on breathing," Davis said.
Giving Narcan is still critical because xylazine is often mixed with fentanyl, and fentanyl is killing people.
"If you see anyone who you suspect has an overdose, please give Narcan," said Bill Soares, an emergency room physician and the director of harm reduction services at Baystate Medical Center in Springfield, Massachusetts.
Soares said calling 911 is also critical, especially with xylazine, "because if the person does not wake up as expected, they're going to need more advanced care."
"Profound sedation" worries health providers
Some people who use drugs say xylazine knocks them out for six to eight hours, raising concerns about the potential for serious injury during this "profound sedation," said Dr. Laura Kehoe, medical director at Massachusetts General Hospital's Substance Use Disorders Bridge Clinic.
Kehoe and other clinicians worry about patients sedated by xylazine who are lying in the sun or snow, perhaps in an isolated area. They could be vulnerable to compression injuries from lying in one position, or they could be attacked.
"We're seeing people who've been sexually assaulted," Kehoe said. "They'll wake up and find that their pants are down or their clothes are missing, and they are completely unaware of what happened."
Kehoe argues that the surge of xylazine heightens the need for supervised consumption clinics, where people can use drugs under the watch of trained staff. Legislation that would have allowed a pilot program in Massachusetts died in committee at the State House this year.
Newton Police Chief John Carmichael, who chairs the Massachusetts Chiefs of Police Association's substance abuse committee, is opposed to supervised consumption. Carmichael says that in his experience, people who buy illegal drugs use them immediately and won't take the time to travel to one of these sites.
"I just don't see how these sites would be really effective," Carmichael said, adding that he'd prefer to focus solely on getting people into treatment. "I think we have an obligation to do that more so."
A study conducted in Vancouver, Canada, showed an increase in treatment as the city added overdose prevention sites.
A recent study out of France found that people who use supervised consumption clinics have fewer boils and abscesses related to injections. Clinicians say that's especially compelling now, with xylazine.
In Greenfield, nurse Katy Robbins pulled up a photo from a patient seen in April as xylazine contamination soared.
"We did sort of go, 'Whoa, what is that?'" Robbins remembered, studying her phone.
The image shows a wound like deep road rash, with an exposed tendon and a spreading infection. Robbins and Tapestry Health have created networks so clients can get same-day appointments with a local doctor or hospital to treat this type of injury. But it is hard to get people to go get their wounds seen.
"There's so much stigma and shame around injection drug use," said Robbins. "Often people wait until they have a life-threatening infection."
That may be one reason that amputations are increasing for people who use drugs in Philadelphia.
"We're certainly seeing a lot more wounds, and we're seeing some severe wounds," said Dr. Joe D'Orazio, the director of medical toxicology and addiction medicine at Temple University Hospital in Philadelphia.
D'Orazio and his colleagues are still trying to figure out why wounds are worse with xylazine use. It could be that they don't heal as quickly because xylazine reduces blood flow. Some patients also report more skin picking with xylazine.
"Almost everybody is linking this to xylazine," D'Orazio said.
This story is from a reporting partnership that includes WBUR, NPR and KHN (Kaiser Health News).
Copyright 2022 WBUR. To see more, visit WBUR. 9(MDAzMjM2NDYzMDEyMzc1Njk5NjAxNzY3OQ001))





