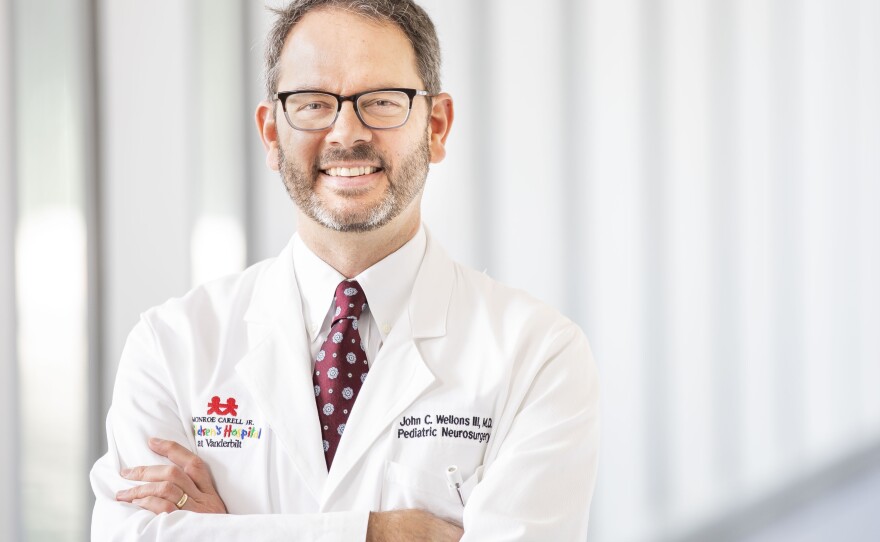
Pediatric neurosurgeon Jay Wellons regularly feels the exhilaration of saving a child from near certain death — and sometimes the anguish of failing to prevent it. He's operated on various parts of the pediatric central nervous system, including performing spine surgery on an in-utero fetus to correct spina bifida.
"Depending on the size of the fetus, [the spine] can be really small, [like] three grains of rice," Wellons says. "We use our magnifying loupes, these surgical loupes, which are magnifying glasses that we wear, and then we have a headlight on so that we can see what we're doing."
Wellons, who's from south Mississippi, says he didn't set out to become a pediatric surgeon. When he first went to medical school, he envisioned himself as a small-town family medicine doctor, who might "occasionally get paid in tomatoes and chickens." But a gross anatomy lab where he learned about the spinal cord and the nerves of the brachial plexus changed his path.
"I remember just spending hours dissecting that out and just being absolutely entranced by it. It was like macramé," Wellons says. "That was the beginning of when I realized that I may be pivoting from a great career in family medicine, which would've been very rewarding, into an entirely different career."
Wellons reflects on his experiences as a pediatric surgeon in the memoir, All That Moves Us. He says he has a big book of photos and mementos from his patients that he pulls out whenever he needs to be lifted up or grounded.
"I will always pull that file out and just flip through it and just think, 'This is why we do what we do,'" he says. "Because it's late nights. It's a lot of hours for the residents and for us in the field. But that degree of gratitude — I mean, I've experienced it as a patient. I've experienced it as a parent, and I've experienced it as a surgeon."
Interview highlights
On how overturning of Roe v. Wade will impact patients whose fetuses have neurological defects
I will tell you a story about my niece and my niece has allowed me to talk about this. My niece ... called me one day after being pregnant for a few weeks to say, 'I'm with the OB, we've just done our 13-week ultrasound and they say that there's a problem with the brain and they say that I need to come see you, Uncle Jay.' And we get her into the fetal clinic, we do the ultrasound. I'm right there with them the whole time — my niece, who I've known since she was a baby, my children walked in her wedding — and there's this encephalocele. It's giant. And the entire brain is on the outside of the skull and it's kind of inverted. So now it's also at the mercy of amniotic fluid, which is that caustic fluid that gets more caustic over time, which is why fetal surgery for spina bifida makes a difference.
So in that scenario, the choices are to have a child that is ultimately born, that's in constant pain, that has no ability to communicate or see or interact with the world around them. They're in a wheelchair, the type of wheelchair that holds your neck still. They have G-tube feedings and over time they never grow up from being a baby. They become adults who have that degree of care that's needed. In situations like this before, with other patients, we've talked about termination and that's what we talked about with my niece. ...
We're going to see a lot more of these now and we're going to have to, as a society, understand that we're going to have to take care of these children. That's our job.
On performing in-utero surgery to correct spina bifida on a fetus
The mom comes into the operating room, she goes to sleep, lines are placed, her stomach is prepped. And then there's an entire team called MFM, the maternal fetal medicine team. ... So the belly is prepped, an incision is made, the uterus is exposed. It's like an orange-pink soccer ball. And the team will ultrasound the dome of the uterus, find a good place to open, make the incision, expose the inside of the uterus, which is where the fetus is. And so, all of a sudden, at, like, 20 to 22 weeks, we're down there looking at this little back that's rotated into place. And at that point is when we do the repair of the back to get that closed in order to reduce some of the long-term sequelae that can occur from spina bifida.
On being a parent and dealing with the death of his patients
I think you have to actively decouple when you're in the middle of it, particularly if you have children and you're a pediatric neurosurgeon. It's almost like I envision myself pressing a clutch to kind of disengage that gear. It's not that easy. ...
[I] kind of have this place that I go to that's just outside of my vision, and it's just kind of a beautiful green field that I think of. I can take kind of the memories and the experience of these [patients] and I can envision myself putting them in a box. It's not like I forget those children. It's just that it's a place that we put them. And I think that's a common feeling among surgeons that deal with things like life and death.
On the importance of communicating clearly with his patients' families
As much as you want to pull the punch, or as much as you don't want to have to be saying it, or as much as you don't think that you could take it if it was being told to you, it's still your job to make sure that they know and they understand. It doesn't mean you can't deliver that without compassion: "I'm so sorry to be having this conversation with you, but your daughter is really sick and we need to get her to the operating room right now." So to some extent, making sure they understand the situation is important, making sure that they understand what the plan is ... making sure they understand what's going on, making sure [they know] what the risks are and then telling them what we're going to do. And then being with them, not stepping away afterwards, going and talking to them after surgery and then, [making rounds] as much as you need to in the ICU, and I think that's critically important as well.
On assault weapons as a public health issue
I've seen some really horrible injuries from gunshot wounds, and it's not specific to assault weapons, but I've seen some injuries to the brain and to the spinal cord leaving a girl paralyzed, quadriplegic on a ventilator. And this has just been part and parcel of a society that has guns in them. ... Nowadays what we see with these assault weapons is that there's so much damage. I have a friend, Jon Martin, who is the chief of pediatric neurosurgery up at Connecticut Children's Hospital. And after the Newtown [Sandy Hook] shootings, he describes them all gowned up and waiting in the hospital for the children to get there until they realized that nobody was really coming because so many people had died. And I just have a hard time understanding why we need these assault weapons within society.
Sam Briger and Seth Kelley produced and edited this interview for broadcast. Bridget Bentz, Molly Seavy-Nesper and Laurel Dalrymple adapted it for the Web.
Copyright 2022 Fresh Air. To see more, visit Fresh Air. 9(MDAzMjM2NDYzMDEyMzc1Njk5NjAxNzY3OQ001))





