Some large health insurance companies have suffered losses under the Affordable Care Act, leading to a few high-profile exits from the health exchanges. Humana is just the latest, announcing in January that it will stop offering health insurance on the Affordable Care Act exchanges at the end of 2017.
But the administrators of a smaller, California-based insurer — Molina Healthcare — managed to turn a modest profit in the early years of the health law. How did they do it?
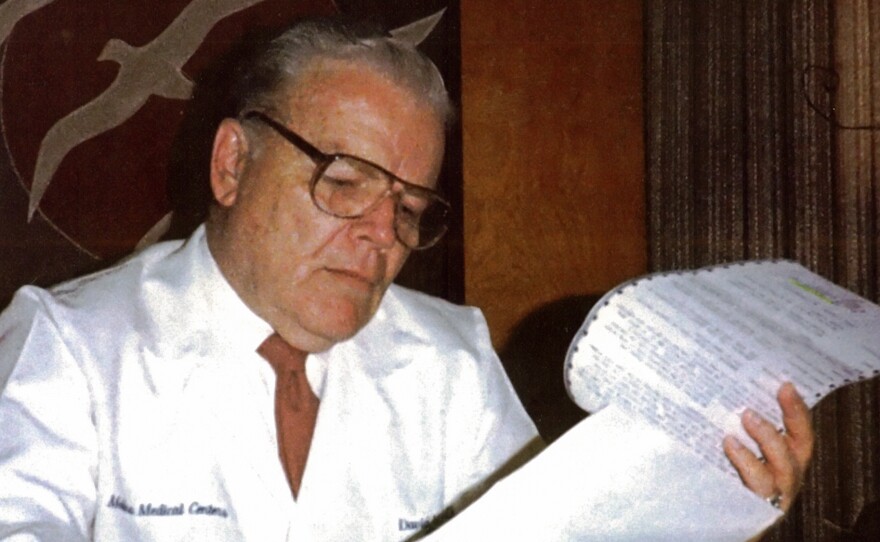
"We understood the demographics of the people that we're serving a little better," says Dr. J. Mario Molina, CEO of Molina Healthcare, "because we've been doing it for so long."
Molina's father, David, also a doctor, first founded a network of medical clinics in southern California in 1980 that served mostly low-income patients. Sometimes when his dad's patients couldn't pay, they would trade services, or give him items from their homes instead of cash, the younger Molina recalls: a glass decanter, a pipe organ, even a dog.
"My father was old-fashioned," says the CEO. "He believed doctors had an obligation to take care of patients, and that the primary issue was not how they were going to get paid."
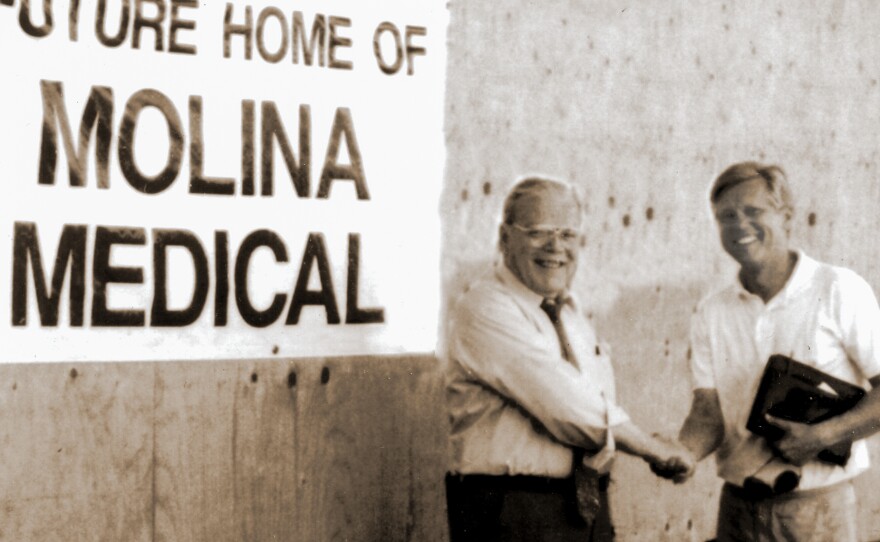
In 1994, David Molina started his health insurance company, focusing on getting care to patients on Medicaid — government health insurance for the poor and disabled.
That is what positioned Molina Healthcare to move into the Obamacare marketplaces so smoothly, Mario Molina says — most people who signed up for Obamacare plans are low-income.
"It's a different population most insurance companies haven't been interested in," he says.
For example, transportation is an issue for his company's customers. They often take the bus to medical appointments, he says, so would rather see a doctor close to home, than at an academic hospital 30 miles away.
"We don't contract with every hospital and every doctor," he admits. "It's not everyone, but it's enough so that you can find a doctor and the hospital and the services you need." His company now operates in 12 states and Puerto Rico.
While some have criticized narrow insurance networks for not offering consumers enough choice, especially of medical specialists, having fewer doctors in the Molina Healthcare network has meant lower costs for the company and its customers. That means the health insurance company has been able to earn a modest profit — roughly 1 percent in the first couple years of Obamacare.
Some larger insurers are accustomed to creating health plans for big companies, who often want more doctors and more benefits included, in hopes of attracting and retaining top employees. But plans like that cost more.
"They're looking at things sort of from the top down, and we're looking at things from the bottom up," Molina says.
He's used to running a low-cost, low-margin business, while big guys like Humana, Aetna and UnitedHealth aren't. Industry analysts say that's why some of the big players lost money with Obamacare.
"It's easier to work up from a low-cost position than it is to work down from a higher-cost position," says Josh Weisbrod,a health care consultant with Bain & Company. "For an insurer that is used to selling employer plans with rich benefit designs and broad networks, it is difficult for them to transition that to a narrow network of lower cost providers."
But Molina says there's been a serious downside to his company's success: a provision of the Affordable Care Act known as "risk transfer." The provision was designed to help insurance companies cover losses if they ended up with a lot of really sick, expensive patients. It works like this: Companies with fewer patients who have a chronic or serious illness pay some of their revenues to the companies that cover more patients who are sick.
It was a fine idea, Molina says, but the formula lawmakers came up with to calculate risk was all wrong.
"Let's put it this way," he says. "Currently Molina Healthcare is returning 25 percent of our premiums to the government, which are then distributed to our competitors. So we are really subsidizing our competitors and helping them, rather than forcing them to compete."
And that is one of the things that hit Molina's bottom line in 2016, resulting in much lower profits than originally projected for the year and a significant fourth quarter loss. Molina complains that the risk formula seems to punish efficiency rather than help those who had some bad luck.
"I think it was done by well-meaning people who had a theoretical knowledge, but not a practical knowledge of insurance," he says.
Still, Molina remains a fan of the Affordable Care Act overall, and hopes Congress will consult with him and other insurers as it debates the future of the health law.
"It doesn't need to be scrapped and replaced," he says. "It needs a tuneup."
If lawmakers need guidance on how to fix Obamacare, he adds, they should look at one state that really got it right: California.
California insurance regulators and health officials "forced everyone to really compete," Molina says, "and that made everyone kind of sharpen their pencils and do a better job," he says. "It's kept everyone on their toes, and, as a result, I think there's been more stability in the marketplace."
There's also more predictability. California may have more business regulations than other states, but Molina believes that's created a level playing field.
"The state doesn't make arbitrary decisions," he says. "We can plan from year to year. We understand the rules. Imagine if you're trying to play a game and the rules change in every quarter."
Molina is hoping newly-elected rule makers at the federal level will take his message to heart, too.
This story is part of NPR's reporting partnership with KQED and Kaiser Health News.
Copyright 2017 KQED Public Media. To see more, visit KQED Public Media.