HIV is sexist.
A woman is twice as likely to catch the virus from an infected partner in a heterosexual relationship than a man is.
And homosexual men are at even greater risk. They're more than 20 times as likely to get infected from an HIV-positive partner than couples in a heterosexual relationship.
Now scientists at Microsoft Research and the Zambia-Emory HIV Project have a clue to why these disparities exists.
Only the strongest, most evolutionary "fit" versions of the virus can successfully infect a man when he has sex with an HIV-positive woman, Jonathan Carlson and his colleagues report Thursday in the journal Science.
In other words, only particular versions of the virus, with particular DNA sequences, can pass from a woman to a man. These reduces the chance an infection occurs during sex.
The restriction is less when women have sex with an HIV-positive man. And, most likely, reduced even further when men have sex with men. So the chance of an infection increases in both situations.
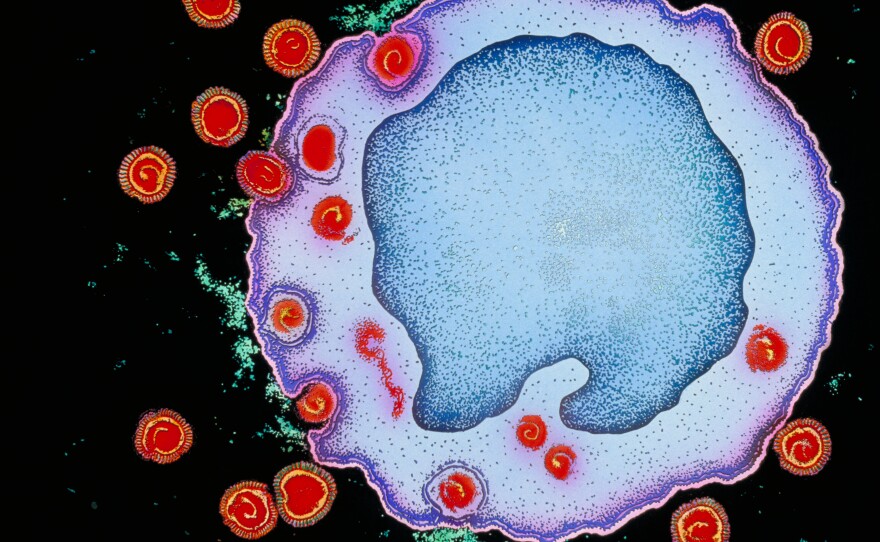
As HIV replicates inside a person, mutations are introduced into its DNA. This results in a large number of different HIV versions swarming about the body — each with its own genetic code.
But when HIV is transmitted through sex, usually only a single version of the virus establishes a long-term infection. So the process is almost like a filter, letting only certain viruses through.
This made Carlson and his team wonder: Is there something special about the HIV versions making it through the filter?
To figure this out, Carlson and his colleagues monitored HIV transmission between "discordant" heterosexual couples in Zambia for a decade. These are couples in which one person is HIV-positive and the other is HIV-negative.
During the experiment, the team gave the couples condoms and taught them other ways to prevent passing along HIV to their partner.
But in 137 couples transmission did occur. In these cases, Carlson and the team compared the viruses of the newly infected person with those of the partner.
They found that HIV was most likely to be transmitted when its genetic code had a particular pattern. These versions of the HIV genes seem to make the virus good at infecting and surviving inside a person's immune system.
Turned out, this pattern is the average DNA sequence that scientists find when they examine HIV strains in people from around the globe. "The average sequence in the population is probably average because it works best, and we found that that is true," Carlson says.
To establish a long-term infection through sexual contact, an HIV virus must first infect a single cell on the genitals. Then the virus multiples and spreads to adjacent cells. "Fitter" viruses are more efficient at infecting new cells and then replicating themselves, Carlson says.
And the higher the initial barrier to this initial infection, the fitter the virus has to be complete this process.
Different parts of the body provide various levels of protection from the virus. The cells on the penis are tougher to infect than those in the vagina or anus. Trauma, such as open sores or ulcers in the genital area, can also increase the chance of infection.
"What was most striking was that risk factors that were known to affect the risk of transmission affected the selection," says pathologist Eric Hunter, at Emory University, who contributed to the study.
They found that viruses in newly-infected men were more "fit" than the viruses in newly-infected women. But when men had genital ulcers or inflammation, they were also infected with less fit versions of the virus.
And though their research was restricted to heterosexual couples, they anticipate that anal sex between homosexual men would provide a lower barrier to infection, and result in the transmission of less fit versions of the virus.
These findings suggest that an effective vaccine might not have to protect against all versions of the virus, just those that are most likely to be transmitted, says Boston University's Manish Sagar, who wasn't involved with the current study.
"You could envision a vaccine that weakens the virus in chronically infected people and needed to be administered only once," he says. "Their disease isn't weakened, but their virus is weakened. So when they have sexual contact, the chance of transmission is lowered."
In other words, this would be a vaccine given to people already infected with HIV to prevent them from spreading the virus.
Copyright 2014 NPR. To see more, visit http://www.npr.org/